Two-Parent Co-Nursing in Queer Families
Bachelor's Research Thesis in Midwifery, 2012
by Jasper Moon
I am happy to email the pdf of this paper upon request.
(Superscript numbers correspond to source citations; asterisks with letters are footnotes for clarification.)

Introduction
"I felt that because I did breastfeed my non-biological child...she has a deeper bond with me. I feel that others saw me breastfeed and it solidified my place as an active mom. Strangers didn't question if I was the bio mom because they saw me feed her." --Julie1
What makes a parent a parent? The parent-child relationship is integral to our society and to our self-identity, so it makes sense we care so much about how to define it. Despite the increasing variety in how families are structured, the hetero-paired nuclear family is often still seen as the standard upon which others are based, and from which they deviate. It makes sense: one mom and one dad, with children biologically descended from both, makes for easily defined familial relationships. For parents who are genetically unrelated to the child, these relationships are no longer seen as absolute, and cannot be taken for granted. We have to discuss them, worry about them, and go to great lengths to protect them. Lacking genetics, we rely on our actions to define us as parents. It is true that some actions are interpreted more unquestioningly as those of a legitimate parent than others, including genetic contribution and legal guardianship, factors over which we may have no control. These actions are not more important to parenting, but because they confer such widely-accepted markers of legitimacy, they function as shortcuts to determining parenthood. I would like to add nursing (also called chestfeeding or breastfeeding, not to be confused with the career of being a nurse) to that list. By sharing the joys and responsibilities of nursing, non-gestational parents can strengthen their familial relationships and declare their legitimacy as parents, to themselves, within the family, and to the world.
Location and Terminology
Because we all write from within our own perspective, it is imperative for authors to discuss their location in relation to the text. My viewpoint is that of an early-30's queer. I was assigned female at birth, though I do not exactly identify as either female or male today; my partner at the time of initial writing identifies as lesbian. I am not yet a parent, so have no first-hand experience co-nursing or nursing in general. (Edit: I became a single parent in 2013 and nursed for two years with the use of at-nipple donor milk supplementation.) I was raised working class on the west coast of the US and am college educated. My studies and career path focus on midwifery and holistic reproductive health. I support nursing and also support parents' innate right to choose what is best for themselves and their families.Though I am aware that preferred terminology varies widely even within communities, and I am unlikely to find a term that makes everyone happy, I intend to use the umbrella term queer for the families kind enough to share their experiences with me. Queer in this sense encompasses partnerships between cis or trans women (who may or may not identify as lesbian, bisexual, pansexual, etc), partnerships between cis or trans men (who may identify as gay, bisexual, pansexual, etc), and/or any relationship in which one or both partners are transgender or genderqueer. I recognize that this working definition must allow room for flexibility, and is not meant to be final. Because family structures can vary immensely, some of the points I discuss may be relevant for your family and others may not. Conversely, I will use the terms straight or hetero-partnered to refer to couples consisting of a cisgender woman and a cisgender man. (I recognize that these folks may also be queer.)
I would also like to emphasize that, though I have not limited my participants to those in dyad relationships, at this point I have not spoken with any three-or-more parent families in which two or more partners have shared nursing. The outcomes of my research should be applicable to polyamorous families, although variables are present and future research should include poly parents when discussing queer families.
In general, I believe that parenthood is not a gendered act, and I will attempt to refer to parents collectively as parents, although some discussion points refer to the sociolinguistic implications unique to mother, and I use the gendered term at that time.
Review of the Literature
Families headed by queer couples are sometimes said to be on the frontier of parenting. Studies have repeatedly found these couples to be more egalitarian when it comes to division of labor, as well as in their roles and responsibilities as parents, compared with their straight counterparts.2,3 Reports of labor ratios across all types of tasks are closer to equal for queer couples than for hetero-partnered couples. Also, whereas straight men believe themselves to be contributing more than their partners report, members of queer couples are more likely to agree about who actually does what work. This indicates that queer couples may be more aware of labor division and be more likely to discuss the division together.Early parenting, however, tends to push even the most egalitarian families toward specialized roles: while queer couples still divide housework relatively equally, birthing parents contribute disproportionately more to childcare, and their partners work more outside the home.4 The largest factor in this division of labor is certainly the nursing relationship: because pregnancy and birth naturally lead to lactation, the parent who gave birth--the gestational parent (GP)--is far more likely to have a nursing relationship with their new baby while the non-gestational parent (NGP) bonds with the baby through other means while providing a larger share of the financial support.
This disparity can lead to complicated emotions for both partners. The GP can become exhausted and overwhelmed, and may be struggling to balance parenting and nursing. On the other hand, the NGP can have mixed emotions about watching their partner breastfeed: they may cherish the closeness shared by two of their favorite people, and at the same time mourn the lack of their own special connection to the baby.5,6(p484) When Goldberg and Perry-Jenkins talked to lesbian couples during pregnancy and then again three months postpartum, the NGPs they interviewed "felt envious of their partner's capacity to nurse, and excluded from the neonatal dyad."4(p310)
This specialization of roles is certainly not unique to queer families. In her blog, Freja writes about her experience being a nursing parent in an otherwise egalitarian relationship:
We were emphatically committed to sharing the duties of parenting. But this [nursing] is something that we cannot share. It does not matter how much of a feminist you are, how committed you are to equal parenting, how dismissive you are of gender roles: if one of you is breastfeeding, [it] will result in you being utterly tied to that child in a way that no one else can share.7Freja's observation reaches across family structures to a problem familiar to many parents, queer and straight alike.
The majority of hetero-paired couples, however, despite any difference in parental roles, have an equality in relationship to the baby that is unattainable for many queer families. When pregnancy occurs "the old fashioned way," both parents will be genetically related to the baby, and even couples using fertility assistance are generally granted automatic legal guardianship. Babies in queer families, on the other hand, are more likely formed with gametes from one of the intended parents and those of a donor, which results in "genetic asymmetry"8(p173) within the family. Although the GP is indisputably the baby's parent, the NGP's status as a true parent is less obvious. In most cases, the legal system considers one the biological parent, and the other, a biological--and thus, legal--stranger to the baby. In about half of the US states, guardianship is granted only after a home visit and expensive second-parent adoption process similar to that of step-parent adoption, despite intending parenthood since prior to conception.9 In other states, same-sex second-parent adoption isn't allowed at all, and parents are stuck in the perilous situation of choosing which parent gets legal protection and the ability to make choices on behalf of their child. This legal situation, and the socio-political climate that reciprocally reinforces it, makes the NGP's role as a parent much more tenuous than the GP or either parent in a heterosexual couple.
Queer parents experience this phenomenon, which I refer to here as gestational privilege, in many ways: NGPs may be barred access to their child in the hospital. Strangers may direct questions about the baby to the GP as if the NGP does not know the answer.*A And in the unfortunate event of a break-up, NGPs may not be granted custody or visitation rights.
The interplay between a queer couple's inclination toward egalitarian parenting and the stressors of genetic asymmetry influence the question of how to become parents in the first place. Goldberg reports that some lesbian couples are specifically choosing adoption because it offers "a unique advantage over insemination, in that it will eliminate the asymmetry of their roles and allow both partners to start out on 'equal footing.'"10(p942) Both parents are symmetrically non-related to the baby, and an equal division of childcare is easy, as parents can share bottle-feeding duties.
Another option for AFAB/AFAB (assigned female at birth) couples is for both to be biological parents to the baby: one as the genetic parent, and the other as the gestational/ birthing parent. This can be accomplished by extracting one partner's eggs, fertilizing them with donor sperm, and implanting them in the other's uterus. The process, which has been called "reciprocal IVF" or "ROPA" (Reception of Oocytes from PArtner), is the same as that used by folks conceiving with the help of an egg donor or gestational surrogate. One article on the ethical implications of ROPA stresses the importance of "contribution of both partners in the creation of the child, the confirmation this entails for their relationship, and the foundation of a shared responsibility for the well-being of the child."11(p814) Essentially, ROPA allows non-gestational parents access to some additional markers of parental legitimacy, and the fact that some families choose to undergo this expensive and medically intensive procedure is evidence of the importance of these markers. The fact that queer families are willing to put in the extra time, effort, and money for adoption or ROPA exemplifies their dedication to strategies supportive of egalitarian dynamics and parental legitimacy.
In a different context, Zizzo also discusses the tenuous nature of the parental role, and ways in which one can acquire markers of parenthood. In her interviews with heterosexual donors and recipients at a milk bank, she found that they frequently had no issue with sharing breast milk...so long as this breast milk was not delivered through breastfeeding or the suckling of another woman's breast... [A] distance from the body that provided the breast milk was preferred, so that emotional bonds between their child and the woman who produced the milk were not formed, thereby, compromising their own maternal identity.12(p103) Zizzo's research corroborates the idea of a strong societal association between nursing and parenthood, which is relatively recent. Whereas the wet nurse used to be commonplace and was not considered threatening to parents, today nursing a baby unambiguously declares one's parenthood.
Other research corroborates Zizzo's hypothesis that the nursing relationship is a key factor in parent-infant bonding.5,6,13 Goldberg, Downing, and Sauck examined the parental preferences of children raised by lesbian couples, as well as the parents' perceptions about why such preferences existed.14 Overall, participants reported that their older children tended to prefer both parents equally, or they alternate in a roughly equal way. However, parents overwhelmingly reported their babies' and younger children's preference for their gestational parent; even more interesting, the parents themselves predominantly attributed this preference to the nursing relationship. In a family in which parity is so valued and genetic asymmetry is likely, a child's strong parental preference can be an added stressor on the family: "the initial preference for the [gestational parent] was indeed a 'problem' that required collaborative work on the part of each parent to make things more equal."14(p426)
A famous example of this stress is entertainer Rosie O'Donnell's announcement on The View that she had pressured her partner Kelli to stop nursing their baby Vivienne: "Kelli only nursed for like a month and then I was very angry. With the other babies, nobody nursed because they were adopted. But with this baby she was the only one getting to bond, so I was like, 'The nursing is over!' I cut her off."15 O'Donnell got a lot of criticism for her comments, but unfortunately not many of the reactions acknowledged how difficult the asymmetrical relationship was for her. Perhaps her approach was severe, but O'Donnell found a way to create new models for parenting that worked for her family.
Knowing that nursing produces distinct roles and relationships, many queer couples have sought ways to apply their more egalitarian parenting style to the supposedly inherent inequity of feeding a baby. Some families create a system for the NGP to feed as well, via some combination of the GP pumping, donor milk, and formula. Then the NGP can feed the baby via a bottle or supplemental nursing system (SNS), a bottle or syringe attached to a tube placed at the nipple so a non-lactating parent can provide nutrition and reap the other benefits of nursing.5,6 Other parents, like Rosie and Kelli O'Donnell, choose to forego nursing altogether, so they can take turns bottle feeding and thus keep parity well-defined.
Each of these strategies allow NGPs to participate in feeding their babies, and many parents who had "the complementary role of bottlefeeding...noted some relief at this arrangement."4(p309) However, there is no tactic that works for everyone. Many parents prefer the baby to be fed human milk over use of formula, and pumping requires a lot of time and effort from the GP--some say even more so than simply nursing.5 For many families, these strategies serve to create a more harmonious household, but a growing minority of queer parents are looking beyond these options, to something that might better fit their needs or goals for parenting.
Queer families seeking alternatives might look to the experiences of another group of parents who share the dilemmas of feeding and bonding with babies they did not birth, as well as the struggles of parental legitimacy: adoptive parents and parents whose babies are born via gestational surrogacy. Like queer parents, these parents may choose to feed their babies formula using a bottle or SNS, but some have decided that their best option is induced lactation, a process by which someone encourages milk production without pregnancy. Inducing lactation involves stimulating the nipples, lacation tissue and endocrine system, usually with a breast pump. Herbs or medications may also be used to increase levels of prolactin, the body's hormone that stimulates milk production.16-19
The most well known protocols for inducing lactation are those created by Jack Newman. In 2000, together with lactation professional Lenore Goldfarb, he developed what became known as the Newman-Goldfarb Protocols to help Lenore nurse her own baby, who was born via gestational surrogacy.17 Their original work has since developed into three different protocols on induced lactation; parents choose from among them depending on their situation. The three protocols vary in details, but generally use birth control pills and Domperidone, in addition to pumping, eating oatmeal, drinking lots of water, and taking the herbs fenugreek and blessed thistle.
If adoptive parents and parents of babies born via gestational surrogacy can induce lactation and nurse their babies, why not the NGP in a queer family? Zizzo proposes that queer couples can "facilitate an equal bond with their child based on the physical act of breastfeeding"12(p104) as well as "equal recognition as dual [parents] from the very early stages of their parenting experience."12(p96) It seems fitting that a strategy available only to queer families could be used to alleviate stressors unique to queer families. Ironically, Zizzo's work is based on interviews with straight-identified donors and recipients of banked milk: her proposal about queer families is only hypothetical.
Although Zizzo never worked with queer parents, Newman and Goldfarb have. Their protocols are easily adapted to a two-parent shared nursing situation, and in fact already have been. In 2007, Goldfarb gave a presentation on induced lactation with several case studies, including a lesbian couple in which the NGP induced lactation while her partner was pregnant, and then both nursed the baby.18 Unfortunately, Goldfarb only mentions a few logistical facts about them on a presentation slide, so it's difficult to surmise how the process influenced their lives.
Through much research and networking, I have been able to contact other families who are willing to speak about their experiences sharing nursing. Some of these queer couples intentionally chose to induce lactation, like Goldfarb's case study parents. Other couples were both already lactating: either they were pregnant at the same time or close together, or they took turns at pregnancy and the NGP of the new baby still had a milk supply from nursing their older child. In order to investigate the nuances of two-parent co-nursing, we clearly need to talk to these families about their experiences. Never before have the co-nursing experiences of queer families been gathered together, and I am excited to have the opportunity to do so.
Research Design
My research explores the effects of co-nursing on division of childcare, familial relationships, and perceptions of parental legitimacy. The research tool consists of an online questionnaire distributed to parents in queer relationships who shared nursing of one or more children with their partners. Because this practice is relatively uncommon, parents were recruited mostly via online networking. An invitation to participate was extended to parents of every known eligible family: a total of 17 parents from nine families.The questionnaire has a core of 30 questions for those with experience co-nursing one child, 13 of which are child-specific, and are repeated for each additional child. The questions cover the following subjects: logistics about the breastfeeding experience, division of childcare, perceptions regarding familial relationships, perceptions of parental legitimacy, and overall opinions on the co-nursing experience.*B Research was conducted in Portland, OR in the winter of 2012; participants were given one week to complete the questionnaires.
Parents were allowed to choose a pseudonym for themselves to provide anonymity. Throughout this paper, all references to participants and quotations will use these self-selected pseudonyms. All research findings and quotations from participants are sourced from my questionnaire, entitled Experiences Co-Nursing in Queer Families1; full participant responses can be found in Appendix B.*C
Research Findings
My initial questionnaire response rate was 88%: of the 17 invitations, I received responses from 15 parents. The day after I closed my questionnaire to responses, I was contacted by another prospective volunteer who, along with her partner, wanted to participate. They both completed the questionnaire, bringing my totals to 17 parents, representing ten families,*D discussing their experiences co-nursing 20 separate children. The majority of parents identify as female; they describe themselves as lesbian, queer, dyke, bisexual, gay, and "currently with a woman." One participant identifies as transsexual male. Racial/ ethnic identification was predominantly white or Caucasian, with two respondents identifying as "white, Hispanic" and three as "white, Jewish"; heritage includes Australian, Cuban, German, and Chilean. Reported economic class backgrounds varied from working class to upper-middle class, with the majority lower-middle or middle class. These families have one to four children and live mostly throughout the US, with two families in Australia. They have experience co-nursing children across a range of years: some still have infants, and others have children who are now adults. The majority (15) of the children who were co-nursed are currently between one and five years old.For some aspects of analysis, I have divided the participants' experiences into categories based on their nursing arrangement. The majority of experiences are of parents cross-feeding their children: I have received 14 accounts of cross-feeding from the NGPs' perspective and 13 accounts by GPs of their partners cross-feeding. These cross-feeding accounts represent six families. Of the four families that induced lactation, I have four accounts of NGPs who induced lactation, including two accounts by an adoptive couple in which both parents induced lactation, and two experiences of GPs whose partners induced lactation. I also have two accounts from a GP whose partner fed the babies using an SNS. One family has experiences with induced lactation as well as cross-feeding.
Account-specific questions. After the demographics questions, parents were asked about their experience co-nursing a given baby. Parents answered this set of questions once for each baby they co-nursed, so some parents provided accounts of their experiences both as a GP and as an NGP, or the experiences with cross-feeding and with induced lactation. Although I find it useful for some analyses to compare average responses by GPs with those by NGPs, I in no way mean to imply that each family has one of each. One really helpful aspect of the way the questionnaire was set up was that when members of a couple both participated, their children were discussed twice: once by each responding parent. This allowed me to compare their perspectives to get a more thorough view of the experience.
For the most part, GPs provided more of the baby's milk than NGPs: 80.0% for cross-feeding families and 87.5% for families inducing lactation. In eight of the ten participating families, the GP contributed at least 60% of the breast milk, except for one NGP who was the at-home caregiver, and contributed 60% herself. The participants who adopted and both induced lactation reported contributing equal amounts of breast milk, and the family that used an SNS reported the baby consumed 100% breast milk from the GP.
Participants recorded their own frequency of nursing as well as that of their partner. In instances in which partners also completed the questionnaire, I received two accounts of the experience, one from each of their perspective (and responses differed from partner to partner). Therefore some situations are recorded twice, one for each parent's experience.
Examining the results of the nursing frequency question,(Figure 1) which is broken into 3-month increments for the first year, I was surprised and proud to see that all 20 of these kids were nursed up to around their first birthday or beyond! This statistic in itself is noteworthy, and suggests a link between the decision to co-nurse and the familial valuing of extended nursing.
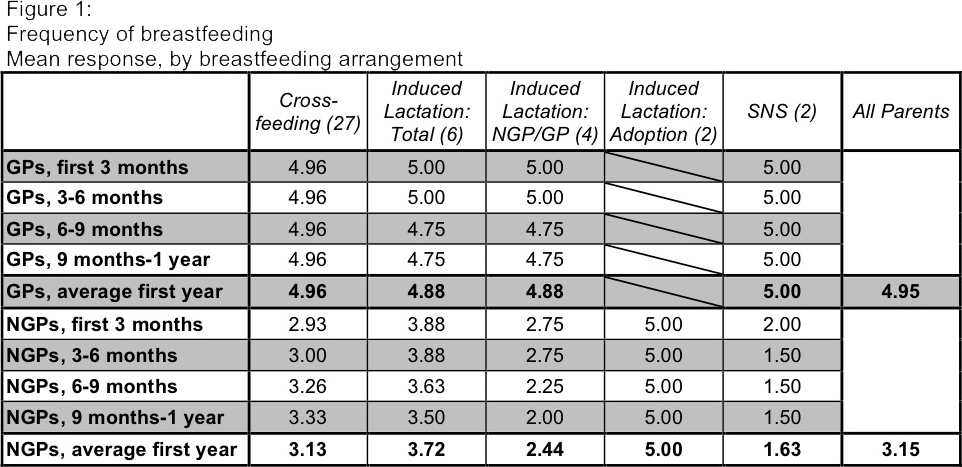
Findings showed a tendency for GPs to nurse more often than NGPs, with most GPs across the board nursing day and night for the duration of the first year. NGPs frequency of nursing varied a lot, and often varied for a given family over the course of the first year. At first glance, it seems cross-feeding NGPs nursed less often than NGPs who induced lactation. However, the participating couple in which both partners induced lactation for their baby, who was adopted, had a vastly different experience from those of other induced lactation families: they both reported nursing day and night for the entirety of the first year, and were the only induced lactation NGPs to have done so. For NGPs who induced lactation and whose partners were GP to the baby, the average frequency of nursing was 2.44. In addition, the cross-feeding group's responses were skewed by several parents who reported nursing "not at all" at first. These parents actually did not begin to co-nurse until their younger children were born, whom they birthed. These few responses shifted the mean frequency down a bit.
Only two participants elaborated on how the specific division of nursing affected them, but their experiences may offer some insight into these numbers. Chloe and Beam, co-parents in a cross-feeding family, both reported attempting a close to 50/50 split of nursing with their first pair of children, born 15 weeks apart. As Chloe described, "we initially started out, and hoped, to share nursing exactly equally. We swapped night feeding from one night to the next (which was stressful). It turned out that this was too hard, both for us and the babies." With their second pair, born 10 weeks apart, Chloe says:
I absolutely insisted that we not swap night feeding at all - my partner was reluctant (because she still believed that we should be able to feed and be attached 50/50) but I wouldn't budge! We still did a fair bit of cross-feeding during the day, more as they got older, and even more once they became mobile. So we ended up with a better outcome than we did when we tried to institute exactly 50/50 feeding!Her partner Beam agreed that they "tried hard to do 50/50 with the first babies... It worked much better when we were more relaxed about our parenting." Chloe and Beam were the only parents to discuss trying different nursing ratios; they were also the only parents who had the opportunity to cross-feed twice. While their experience is only their own, potential co-nursing families may be relieved to hear that they found the "more relaxed" approach worked better. Perhaps less concern about doing things "exactly equally" leads to less stress over all.
In general, the questionnaire results do indicate that co-nursing is somewhat less stressful than without co-nursing, a mean of 5.0 on a 7-point scale, with 1 being much more stress than without co-nursing, 4 being about the same amount of stress, and 7 being much less stress. 5 on this scale was marked "somewhat less stress." Analyzed based on nursing arrangement, accounts of GPs whose partners induced lactation found the situation the least stressful at a mean of 5.5; their counterparts, NGPs who induced lactation, found it more stressful than their partners, but still less stressful than without co-nursing, at 5.0. There was a smaller discrepancy between cross-feeding partners: NGP cross-feeders reported 5.16 and GP cross-feeders 5.09. The only group that reported co-nursing to be more stressful than without co-nursing was the SNS group, with a mean response of 3.*E The parent who reported these experiences attributed the added stress to the work of pumping, using an SNS, and cleaning up. Only one other participant reported co-nursing to have been more stressful: she indicated a stress level of 2 with her oldest two children (similar age, cross-fed), but she also reported it was less stressful with her younger two children (also similar age cross-fed). Overall, co-nursing appears to have a stress-reducing effect on the family.
Perhaps the most important findings in the analysis of specific co-nursing accounts are those about how parents perceive co-nursing to have affected their familial relationships. Participants were asked about their own relationship with the baby, their partner's relationship with the baby, and their relationship with their partner: they rated each relationship "within the first 6 months" as well as the "long term relationship." Responses fell on a scale of 1-100, with 1 being "Weaker/ More Distant," 100 being "Stronger/ Closer," and 50 being "Not Affected at All."
The first thing I noticed was that nearly everyone reported all relationships at 50 or greater, meaning that overall, they felt co-nursing was beneficial or neutral.(Figure 2) Of the six relationship assessments for each of 35 co-nursing experiences (210 total responses), only three fell on the "weaker/ more distant" end of the scale, at less than 50. These ratings were 46, 45, and 29, and they each related to specific difficulties the families were experiencing at the time. I found this positive response very encouraging.
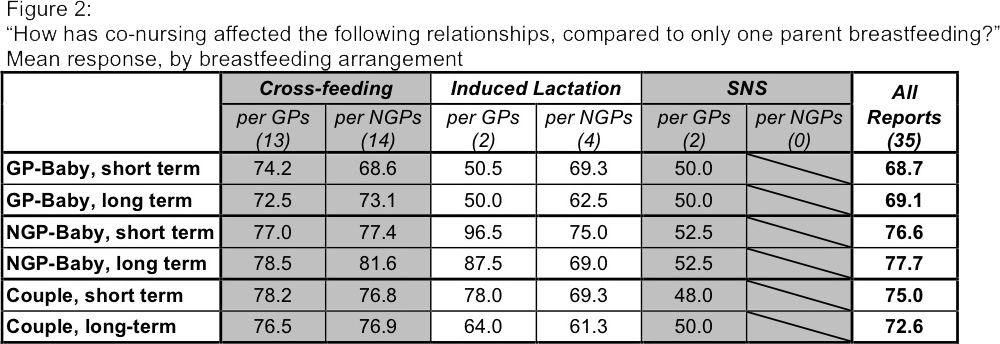
After initial evaluation, I grouped responses of the NGP-baby relationship, GP-baby relationship, and the couple's relationship, and further divided responses based on whether they were cross-feeding, induced lactation, or used an SNS. I was not surprised to find that everyone found co-nursing to be more beneficial to NGP-baby relationships than to GP-baby relationships, considering the default alternative is for the GP to nurse the baby alone.
One noteworthy difference between groups is the effect of co-nursing on the GP-baby relationship. Gestational parents whose partners induced lactation reported co-nursing to have little to no effect on the GP-baby relationship (50.5 in the short term and 50.0 in the long term); the participant whose partner used an SNS also reported no effect on the GP-baby relationship. However, gestational parents whose partners cross-fed reported co-nursing to have a marked benefit for the GP-baby relationship (74.2 in the short term and 72.5 in the long term). One potential explanation for this is the added relationship with the other baby. Within induced lactation couples, both GPs and NGPs were more likely to report more benefit to their partner's relationship to the baby than their partners reported themselves.
Cross-feeding couples also reported higher benefit to their partner relationship: both NGPs and GPs average about 77 for both the short and long term. Induced lactation couples also saw a partner relationship benefit, although slightly less than the cross-feeding group, with GPs reporting higher levels of benefit (78 in the short term, 64 over time) than NGPs (69.3 in the short term, 61.3 over time).
Some participants elaborated on the benefit of strengthening relationships, especially the relationship between babies and NGPs. As Anne says, "[m]y partner had some problems bonding well with her, and I think knowing she can breastfeed her, helped her move through that." Ruth responded similarly: "while breastfeeding is not the only way to bond with a child, it is a powerful way, and it helped my wife bond with our daughter in a special way."
General opinion questions. The final set of questions was only asked once per participant, regardless of their situation. These were primarily looking at overall feelings about co-nursing, as well as a matrix about perceptions of parental legitimacy. This section also included several open-ended questions, including some that allowed participants to elaborate on other questions as they liked.
Out of the entire questionnaire, the question with the widest variance was the seven-point scale asking participants to rate whether they found co-nursing from 1, "difficult at first," to 7, "easy at first," with 4 being neutral.(Figure 3) Though the mean value was 4.5, responses were distributed across the range. Looking more closely, we see that responses aligned strongly with breastfeeding arrangement. Mean response for cross-feeders was a rather high 5.5, compared with 2.8 for the induced lactation group and 3.0 for the one parent using an SNS. This response pattern makes a lot of sense, as these arrangements do require a lot more effort than cross-feeding.
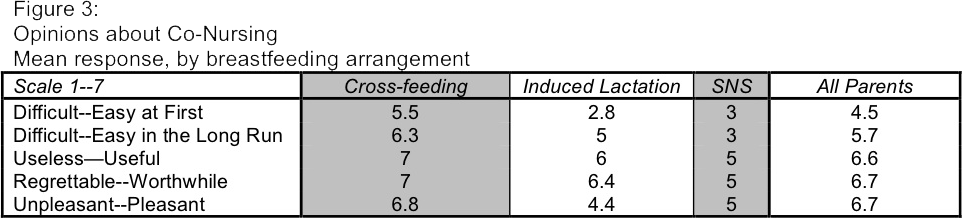
Edit: the actual value for the Induced Lactation group, for the Unpleasant--Pleasant, is 6.8. I have fixed this in the pdf but have not yet changed this .png.
In the long run, co-nursing was easier for almost everyone. The mean response value for "difficult in the long run" to "easy in the long run" was 5.7 on the same seven-point scale. Again, responses were distributed across most of the range, but clustered more toward "easy." Divided into groups based on breastfeeding arrangement, the cross-feeding group again found co-nursing to be easiest, with a mean response of 6.3. The induced lactation group's mean rating rose to 5.0, and the SNS group maintained a 3, which is consistent with the level of work involved.
The other three scales offered to participants had a much clearer response, which varied much less based on nursing arrangement. Parents rated co-nursing a 6.6 on the scale of "useless" to "useful," with 12 parents reporting a 7. The responses on the scale of "regrettable" to "worthwhile" and the scale of "unpleasant" to "pleasant" were identical, with a mean response of 6.7, and 13 parents reporting a 7 for each. No one reported less than a 5 for any of these three values. It is also of note that all 11 members of the cross-feeding group rated co-nursing a 7, the highest possible score, in terms of being useful and of being worthwhile.
To rate perceptions of parental legitimacy, participants were given another seven-point scale. They were asked to report how an NGP, an NGP's partner, extended family, and the general community would view a co-nursing NGP, both in the early months and over the long term.(Figure 4) The scale went from "much less like a 'real' parent" at 1 to "much more like 'real' parent" at 7, with 4 being "the same as without co-nursing."
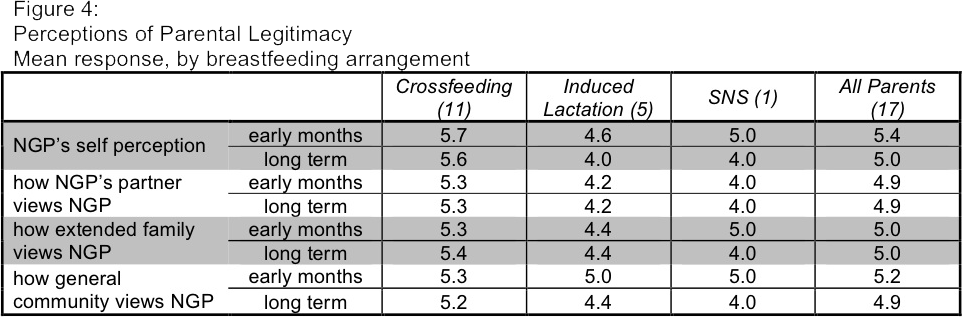
An analysis of the answers to this question suggests that nursing does actually confer some parental markers for NGPs, both within the family and outside: the mean for each category falls between 4.9 and 5.4. Similarly to the relationship-strengthening effect we reviewed earlier, most participants found this effect to be strongest in the early months, and then less so over the long term. Many parents reported increased legitimacy in the early months and then perceptions returning to "the same as without co-nursing" over the long term. Triomami put this well when she says, "I think in the beginning it does make you feel like more of a 'real' parent. I think this effect lessens with time in that regardless of [nursing], you...feel like a real parent when you are in the daily grind. However I think it does mean something to extended family and the community when you are the parent provid[ing] your child (nongestational) with breast milk."
Here, also, we see the clearest correlation in the cross-feeding group. Their mean reported values ranged from 5.2 to 5.7, whereas the mean of the induced lactation group and the SNS participant had values between 4.0 and 5.0--still indicative of increased perceptions of parental legitimacy, but not as markedly as the cross-feeding group.
Many of my participants elaborated on their belief that co-nursing increases perception of an NGP being a "real" parent. As Christy put it, "I consider my kids to each have 2 parents. I have always considered their mama to be their mama...Being able to comfort her child made more people feel like she was a real parent." Particularly interesting is that the strongest legitimizing effect seems to be to the NGPs view of themselves as "real" parents. This could be related to the closer NGP-baby relationship, although whether one causes the other is not within the scope of this research.
When asked about "the strongest benefits of co-nursing," 12 participants included some variation of bonding, intimacy, or closeness to the baby. Eight participants mentioned increased parity, either in the ability to share childcare responsibilities, or babies' ability to be comforted by either parent. Nine listed various factors of convenience or logistical ease. Four parents also mentioned health benefits to the baby, including wider range of antibodies, and two parents each mentioned the fun of it and having a shared experience with their partner.
These open-ended responses help illuminate what factors are most important to families, and corroborate the statistical data from the closed-ended questions. The participants' focus on relationships and parity are especially pertinent. Clearly, participants' emphasis on bonding in the free-write benefits section parallels the closer NGP-baby relationship reported earlier by numeric values, and some of the other responses, especially parity and shared experience, may explain the closer couple relationship values as well.
When asked to discuss "the strongest drawbacks of co-nursing," the trends were less obvious. Six parents said they experienced no drawbacks at all, which in itself is noteworthy; of the 11 who did list drawbacks, four mentioned that co-nursing can be logistically challenging, including two who specifically indicated the time involved with pumping. Three parents listed concern about milk supply issues. Two parents discussed that imbalances can be emotionally difficult: one parent experienced insecurities around baby preferences, and another said "if one parent does it more 'successfully' than the other...then it's stressful." Other issues, mentioned by one participant each, were societal views and the challenge of night weaning when both parents are nursing. One respondent, Kelly, answered, "[t]he unfairness of it. I think sometimes my partner was sad that she didn't breastfeed our first child and she was a little sad that I *could* breastfeed her gestational baby, our second child." Her response indicates the complexity of emotions parents may experience, and suggests that periodic discussion around all of these potential challenges may be required.
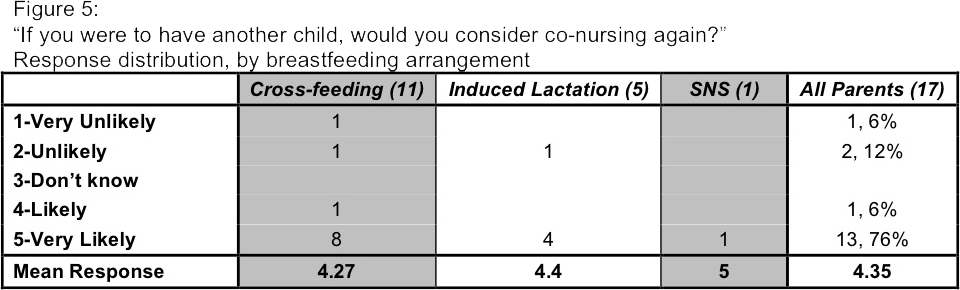
Of the 17 parents, 14 (82%) said they would be "likely" or "very likely" to attempt co-nursing again, with 13 reporting "very likely."(Figure 5) One of the three who said they would be unlikely to co-nurse again, Tracy Linkletter, is an NGP who induced lactation. She says, "I think the experience of co-nursing was wonderful, but I wouldn't do it again because of the difficulty." The other two who would be unlikely to co-nurse again are actually partners: Layla says she "[w]ould not co-nurse again only due to logistics in making my own milk." Her partner, Triomami, adds that she "would totally induce lactation" if her partner were to birth another baby, but she herself would be the one to carry any future children, and her partner would not want to induce lactation.
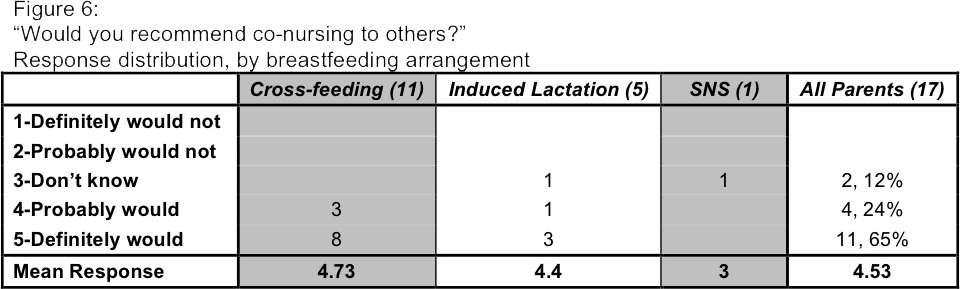
When asked if they would recommend co-nursing to others, 11 of the 17 (65%) "definitely would," and four (24%) "probably would."(Figure 6) The remaining two respondents said they "don't know." No one said they would not recommend it, although some parents mentioned in the free-write section that they do not recommend 50/50 co-nursing.
My participants' answers indicate unmistakably that their overall experience with co-nursing has been positive. Both their numeric ratings and their free-write responses demonstrate the strongest benefits to be in the areas of bonding, logistical ease, and perceptions of parental legitimacy. I would like to express my appreciation for the parents who shared their life experiences for the purpose of this research.
Discussion
Though my findings have been encouraging, more research is clearly indicated. This study had a small sample size of 17 participants, which cannot produce statistically relevant results. I also only collected data from parents who chose to co-nurse. Because one cannot look at the same dyad relationship both with and without co-nursing, I opted to have the parents give their opinions about how these relationships compare to the situation if they had not co-nursed. If I were looking for objective data about relationship strength and closeness, I might have had a control-matched group of parents who did not co-nurse; however, I am actually interested in the subjective opinions of my participants. Regardless of whether the relationship is objectively stronger, I believe that the parents' perception of this strength is actually more important.My research includes families that cross-fed and those that induced lactation, as well as one family that pumped and used an SNS: this variety is both a strength and a limitation. I am able to compare these groups, and my findings are applicable to more families. However, because I included such a variety of arrangements, the statistical significance within each sub-section is even lower, even to the point of having a sample size of only one family.
Another limitation in comparing family nursing arrangements was the difference in number of accounts. Though six families had cross-fed at least once, and four families had induced lactation at least once, the total accounts about cross-feeding (27) were far more numerous than those of inducing lactation (5). I see two factors contributing to this discrepancy. First, both parents from each cross-feeding family completed the survey, whereas three of the induced lactation families ultimately had only one parent participate. Secondly, cross-feeding by definition requires two children, and if the cross-feeding is bi-directional (as it was in every family with similarly aged babies, and some families with an age gap), twice as many experiences are collected.
In terms of my research tool, I might not create questions using sliders again. I don't think they interfered with the data, but it was more difficult to talk about participant responses than the questions that had a selection of choices. I would also have liked to conduct open interviews in addition to the specific questions included in my questionnaire. Family experiences are often so much richer than numbers and little tick boxes can capture.
Recommendations
My primary recommendation is that care providers who work with queer and trans families should be aware of specific emotional, social, and legal issues they may encounter, and keep in mind that families may choose to co-nurse. One of my participants, Beam, tells about her experience with lack of care provider awareness, and perceptions of parental legitimacy: "[d]espite cross feeding, people were still always handing the baby back to my partner. The first day she was born, several midwives were shocked to see me giving her a feed (just colostrum - I was pregnant), and I guess I felt embarrassed too. Less legitimate. Like I shouldn't be feeding her as I wasn't the 'proper' mum." As midwives, we strive to avoid contributing to parents' feeling "embarrassed" and "less legitimate": awareness about co-nursing can help us better support our clients and encourage them as parents.Knowledge of induced lactation protocols is obviously helpful. Some lactation consultants have acquired relevant experience working with adoptive parents or intended parents working with a gestational surrogate, and can apply that experience to their work with queer families. Midwives, on the other hand, rarely work with soon-to-be parents who are not themselves pregnant, so our lactation knowledge focuses on gestational parents nursing newborns, and occasionally working with gestational surrogates or birth mothers who choose adoption: situations that may indicate an opposite protocol, cessation of lactation in the early postpartum. For this reason, midwives, especially those working with queer clientele, should acquire a basic knowledge of the protocols for induced lactation.*F
It is important to remember that there are many possible arrangements for co-nursing. Let the parents tell you their goals and offer to assist in creating a strategy. If working prenatally with a couple in which the NGP is inducing lactation, discuss how the process is going at each prenatal, and provide referrals for access to pharmaceuticals if desired. When discussing the birth plan, include questions about when the NGP intends to begin nursing, and make sure the whole care team is aware and supportive of their plans.
During the postpartum period, remember to inquire about nursing issues for both parents, as well as any emotional issues that may arise, such as insecurities or mourning the loss of co-nursing previous children. Consider creating a list of lactation consultants and nursing support groups with more co-nursing experience.
Conclusion
So, what makes a parent? It's in the little daily things, like bedtime rituals and care for a skinned knee. It's the cuddles, the holidays, and the love: in short, being a parent is what makes a parent. But being a parent can also be really difficult, and we have seen that queer families have unique challenges. The parents who participated in my research reported that co-nursing strengthened familial relationships, eased logistical difficulties, and increased perceptions of parental legitimacy. Overall, they would co-nurse again, and would recommend it to other families. Co-nursing should be seen as one more possible way to bring families together.Footnotes
*A This situation is not specific to queer families; cisgender heterosexual dads, even those genetically-related to their children, report similar experiences, possibly in relation to gender-based assumptions about parenting.*B A copy of the questionnaire is included as Appendix A.
*C One participant opted not to be included in the appendix; the other 16 agreed to be included.
*D Although two volunteers ultimately did not complete the questionnaire, both of their partners did, so have some information from each invited family.
*E The SNS group consists of one participant's experiences with two children.
*F For possible resources, see References 9 and 16-19.
References
- Moon J. Experiences Co-Nursing in Queer Families. Questionnaire. Portland, OR; March 2012.
- Patterson CJ, Sutfin EL, Fulcher M. Division of labor among lesbian and heterosexual parenting couples: correlates of specialized versus shared patterns. Journal of Adult Development. 2004;11(3):179-189.
- Wilson S. Mommies know best. Portland Monthly. September, 2008:95-104.
- Goldberg AE, Perry-Jenkins M. The division of labor and perceptions of parental roles: lesbian couples across the transition to parenthood. Journal of Social and Personal Relationships. 2007;24(2):297-318.
- Aizley H, ed. Confessions of the Other Mother: Nonbiological Lesbian Moms Tell All! Boston, MA: Beacon Press; 2006.
- Brill S. The New Essential Guide to Lesbian Conception, Pregnancy & Birth. New York, NY: Alyson Books; 2006.
- Freja. Breastfeeding. Polyamorous Parenting website. January 8, 2012. Available at: http://polyparenting.blogspot.com/2012/01/breastfeeding.html. Accessed January 18, 2012. [No longer seems to be available.]
- Ehrensaft D. Just Molly and me, and donor makes three: lesbian motherhood in the age of assisted reproductive technology. Journal of Lesbian Studies. 2008;12(2-3):161-178.
- Lambda Legal. Adoption and Parenting. Website of Lambda Legal: Making the Case for Equality. Available at: http://www.lambdalegal.org/issues/adoption-and-parenting. Accessed February 1, 2012.
- Goldberg AE, Downing JB, Richardson HB. The transition from infertility to adoption: perceptions of lesbian and heterosexual couples. Journal of Social and Personal Relationships. 2009;26(6-7):938-963.
- Dondorp WJ, De Wert GM, & Janssens PMW. Shared lesbian motherhood: a challenge of established concepts and frameworks. Human Reproduction. 2010;25(4):812-814.
- Zizzo G. Lesbian families and the negotiation of maternal identity through the unconventional use of breast milk. Gay & Lesbian Issues and Psychology Review. 2009;5(2):96-109.
- Pelka, S. Sharing motherhood: maternal jealousy among lesbian co-mothers. Journal of Homosexuality. 2009;56(2):195-217.
- Goldberg AE, Downing JB, Sauck CC. Perceptions of children's parental preferences in lesbian two-mother households. Journal of Marriage and Family. 2008;70: 419-434.
- O'Donnell R. Cited by: World Entertainment News. Rosie O'Donnell halted her partner's breastfeeding. Hollywood website. June 9, 2005. Available at: http://www.hollywood.com/news/Rosie_ODonnell_Halted_Her_Partners_Breastfeeding/2441315. Accessed August, 2018.
- Bryant C. Nursing the adopted infant. Journal of the American Board of Family Medicine. 2006; 19(4):374-379.
- Newman J, Goldfarb L. The protocols for induced lactation: a guide for maximizing breastmilk production. Ask Lenore website. 2002. Retrieved from www.asklenore.info/breastfeeding/induced_lactation/protocols4print.shtml. Accessed August, 2018.
- Newman J, Goldfarb L. Induced lactation and relactation. Presented at Gold '07 Global Online Lactation Discussion. Ask Lenore website. June 25, 2007. Available at: asklenore.info/breastfeeding/pdf/gold07goldfarbpresentation.pdf. Accessed August, 2018.
- Newman J, Pitman T. Special situations: adoption, breast surgeries, relactation. In: Newman & Pitman's The Ultimate Breastfeeding Book of Answers: The Most Comprehensive Problem-Solving Guide to Breastfeeding from the Foremost Expert in North America. Revised and Updated Edition. New York, NY: Three Rivers Publishing; 2006: 255-269.